Deep Brain Stimulation (DBS) has been approved for the treatment of Parkinson’s Disease (PD), Essential Tremor and Dystonia for a decade in the United States and more recently to treat Obsessive Compulsive Disorders (OCD). The movement disorder program at UPMC now has an experience of treating over one hundred PD patients all of whom have optimally placed DBS electrodes and all of whom have benefited from DBS therapy.
We have reported several factors that are associated with good clinical outcomes in DBS therapy including the DBS electrode being well-placed as well as patient age at the time of DBS implantation. For example, younger patients with a dominant symptom of rigidity have significantly improved rigidity at one year after surgery compared to older PD patients. In contrast, older PD patients with dominant dyskinesia symptoms have more improvement with DBS therapy compared to younger PD patients with dyskinesia.
There is yet little long-term follow-up data looking at outcomes of DBS therapy in dystonia although the data to date shows considerable promise of DBS therapy, especially in children where the target structures are smaller than in adults and require very precise DBS electrode placement. We also previously reported on implanting the youngest known patient to receive DBS implants for the treatment of dystonia.
The DBS device is comprised of two components, a DBS electrode that is permanently implanted into the target structure in the brain and a battery pack or Implanted Pulse Generator (IPG) that is inserted like a pacemaker into the chest.
Typically, DBS surgeries are performed in two stages, one to implant each component. In Stage I, the DBS electrode is implanted into the target structure which depends on the clinical condition being treated. The two deepest targets are in the basal ganglia, which lie at the base of the brain. In Dystonia, the focus is on the Globus Pallidus (GP), and in PD the target is the Sub Thalamic Nucleus (STN).
In most patients, the DBS electrode is implanted on both sides in a surgical procedure in which the patient remains awake treated with local anesthesia of the scalp. Altered levels of activity in the basal ganglia structures that comprise the motor system are the hallmark characteristic of all movement disorders. Implantation of DBS into the target structure and subsequent application of trains of electrical stimulation significantly reduce patient symptoms and augment the ongoing medical management of these disorders.
Although the mechanisms underlying DBS treatment remain poorly understood, DBS is known to act by reducing the high levels of inhibitory neuronal discharge signals that occur in the deep motor nuclei of movement disorder patients, an inhibitory signal that is associated with delayed movement initiation and with slow and shuffling gait. Additionally, DBS also functions to restore the normal patterns of neuronal discharge arising from these structures that left untreated result in unbalanced motor signals that are evident as tremors and shaking.
One key to successful DBS surgery is to place the DBS electrode within the target structure (GP or STN) in a location where the DBS electrical pulses activate the intended target structure alone without spreading electrical current to adjacent neural structures which would result in adverse effects being recorded. For example, a misplaced DBS electrode could cause increased motor contractions or cause altered sensations to occur such as somatosensory parasthesia or visual field phosphenes, etc.
Although initial DBS targeting always uses brain imaging in order to determine the three-dimensional stereotactic coordinates of the target structure in the brain, there are several issues that require perfect targeting to be a requirement for successful DBS therapy.
The first issue is that both the GP and STN are relatively small anatomic structures of about 5 mm x 10 mm x 5mm that lie 120 mm below the skull. In surgical planning, a trajectory is determined that starts at a point outside of the head and ends within the estimated center of the target structure. This trajectory can be thought of as having a cone shape where the cone base is the width of the target of about five mm. Any trajectory through the brain that remains within the cone will place the DBS electrode inside the target. However, for a tract to completely miss the target, the angular deviation (error) from the cone-shaped path need only be 2.4°. This is a small error that can easily be accounted for by small compounding errors in radiology imaging, stereotactic registration and anatomical factors that will vary from patient to patient that could result in a planned trajectory missing the target structure.
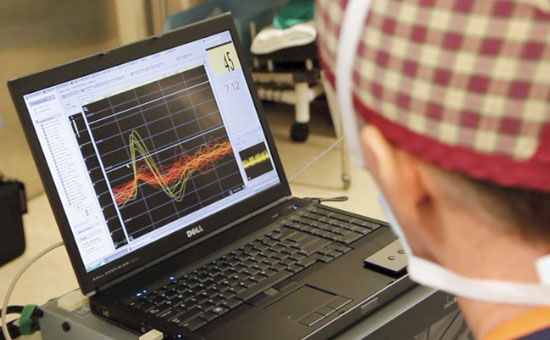
A second issue is that the four-contact DBS electrode is a few mm longer than the target structure so that some part of the DBS electrode cannot be placed inside the target structure. These anatomical and electrode scale factors combine so that accurate DBS placement requires direct confirmation of the electrode tip being placed centrally within the target so that the electrode tip is at the base of the target which means that a portion of the electrode remains above and outside of the target. The neurophysiological technique of microelectrode recording (MER) of single neuron activity is used as an adjunct approach to ensure that the DBS electrode is correctly placed within the target structure. MER involves the placement of a fine micro-electrode wire along the planned trajectory to the target. The micro-electrode is advanced using a fine resolution microdrive until it enters the target structure where neuronal activity is recorded. MER records the discharge patterns of single neurons that identify and confirm the location(s) of neurons within target structures. Characteristic patterns of neural activity produced by single target neurons have been associated with GP and STN as well as other adjacent neural structures such as the thalamus and Substantia Nigra. For example in PD, characteristic patterns of “burst” activity are recorded from STN neurons while in Dystonia, characteristic sustained high frequency neuronal discharge is recorded from GP neurons. By repeatedly recording from neurons and advancing the micro-electrode, the neurophysiology is used to identify each structure and to map its dimensions. Finally, the DBS is placed at specific coordinates revealed from the neurophysiology using the same positioning microdrive.
MER is done with the patient awake and interacting by performing various motor and speech tasks so that the neurophysiological mapping of the target is enhanced by functional mapping to better localize DBS placement within the target. By following up with patients undergoing DBS programming and evaluating their benefits from DBS therapy some correlations have been made between the location of the most effective of the four DBS electrode contacts used for stimulation to achieve the best treatment outcomes. Several reports have indicated that stimulation through contacts placed in the dorsal and posterior quadrant of the STN achieve the most optimal therapeutic results. Additionally, neurophysiological mapping has identified that electrodes placed within STN in locations with identified “kinesthetic” cells, are associated with good clinical outcomes. Kinesthetic cells are neurons whose activity can be modulated through active and passive joint manipulations as identified through functional testing in awake patients.
Through the use of advanced imaging and MER, UPMC movement disorder patients can be assured of receiving DBS implants that are well placed and that provide for optimal post-operative programming of the DBS.
