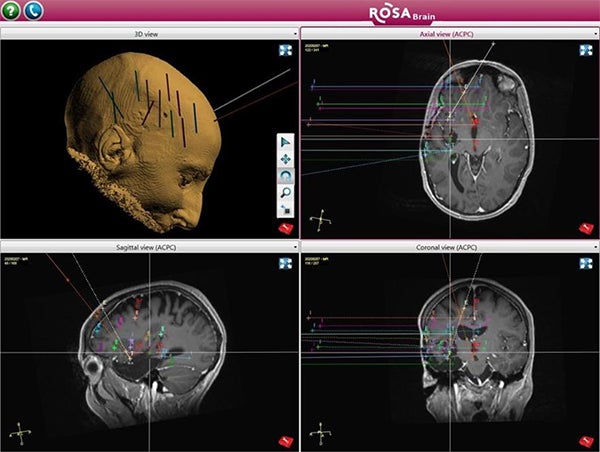
SEEG is the surgical implantation of electrodes into the brain in order to better localize the seizure focus. At UPMC, we use robotic assistance with ROSA® to accurately and efficiently place the electrodes for seizure mapping. Dr. Gonzalez was the first epilepsy surgeon in the US to offer SEEG and has performed over 1000 cases. He is also a pioneer of robotic-assisted neurosurgery, which improves accuracy and shortens surgery time.
Why is SEEG necessary?
The testing you have had so far has helped us gather important information about where in your brain your seizures are coming from, but we have not been able to pinpoint the exact spot. We need to do a diagnostic surgery, called SEEG, to determine the precise location. An analogy is that through your non-invasive testing, we have found the zip code of your seizures, but before we can proceed with surgery, we must also find the street and house number of where your seizures live. SEEG can help us with that.
How is SEEG performed?
We are going to place several (~10-15) electrodes into your brain. These electrodes are thin, floppy wires about the thickness of a spaghetti noodle. We will put the electrodes into the brain areas where we suspect seizures might be starting. To insert each electrode, we will make a small incision in the skin and a small hole in the bone, just big enough to pass the electrode. Each electrode is held in place by a bolt that attaches to the bone. You will not see the bolts or the electrodes as your head will be wrapped with a bandage through the entire hospital stay.
The surgery takes 1-2 hours and you will be asleep the entire time. After surgery, you will get a CT scan and then be transferred to the Epilepsy Monitoring Unit (EMU). The goal is to record seizures just as we did with your previous EMU admission, only this time, you will have electrodes recording from the brain itself instead of from electrodes glued to the skin. Having the electrodes in your brain gives us a “high-definition” EEG and can provide more precise localization of your seizure onset than the scalp electrodes.
What can I expect in the EMU?
This admission will be similar to your previous EMU stay. You will be confined to the hospital bed the entire stay except to use the bathroom. You should bring entertainment with you- books, games, computer/tablet. There is Wi-Fi in the hospital. You may also want to bring underwear, comfortable pants, and some personal hygiene items, although the hospital is able to provide these things to you as well.
While you are in the EMU, we will gradually reduce your seizure medication in an attempt to capture seizures. The plan is to monitor you for about a week, but your stay could be longer, or rarely shorter. It depends on how long it takes to record a seizure, or often more than 1. We also perform some brain mapping during your stay. This involves passing a small electrical current through some of the electrodes, which can help us map important brain functions such as speech. Sometimes this mapping can provoke a seizure, which also provides important information about where your seizures may be coming from.
Will I have pain from SEEG?
No surgery is without pain. You may experience a headache or sensation of pressure in your head, but most patients report this to be mild. You may also experience some jaw pain, pain with chewing, or difficulty opening your mouth wide. We will give you pain medication as needed to make you comfortable.
What is done with the information collected during my admission?
Once we have recorded seizures and performed mapping if needed, the results will be discussed at our patient management conference. Our entire epilepsy team will extensively review the data collected and reach a group consensus about the next step in your treatment. We will discuss our findings and recommendations with you after this meeting. We will schedule you for removal of the electrodes typically the next day.
How are the electrodes removed?
Removal of the electrodes takes about 15 minutes and is performed in the operating room under light sedation. You will be kept overnight for observation and discharged home the following day.
What comes after sEEG?
The goal of SEEG is to better localize your seizure onset so that we can offer you a surgery to stop or reduce your seizures. The recommendation from our patient management conference will be discussed with you before you go home when possible. You will follow up with the surgical team 2-3 weeks after surgery to make a plan for this surgery. We recommend waiting about 4-6 weeks after SEEG before proceeding with the next phase.
Options for epilepsy surgery include: craniotomy for removal of the seizure focus, laser ablation of the seizure focus, and neuromodulation including RNS, DBS, and VNS. If we are able to pinpoint the part of your brain causing seizures, removing that area through a traditional open surgery (craniotomy) offers your best chance for seizure freedom. If your seizures are coming from more than 1 area, a large area, or a brain area that we cannot safely remove, you may be a candidate for neuromodulation (a brain stimulator).
What are the risks of sEEG?
The risk of SEEG is low at ~1%, but no surgery is without risk. There is a risk of bleeding and infection. There is also a chance that despite our best efforts, we cannot localize the part of your brain responsible for seizures.
